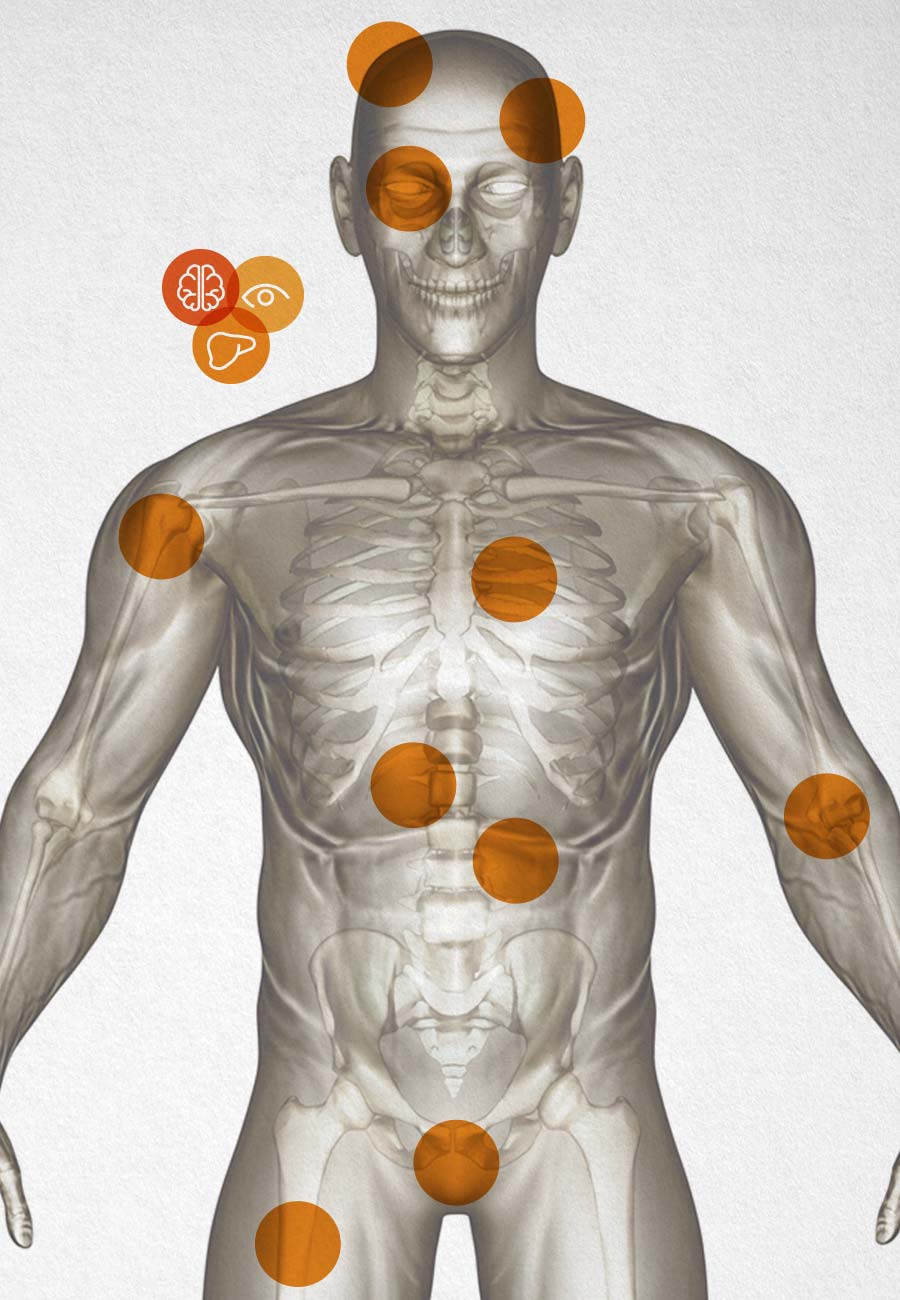
Overview of Wilson disease manifestations
Wilson disease can affect multiple organ systems, including:1-3
- Hepatic
- Neurologic
- Psychiatric
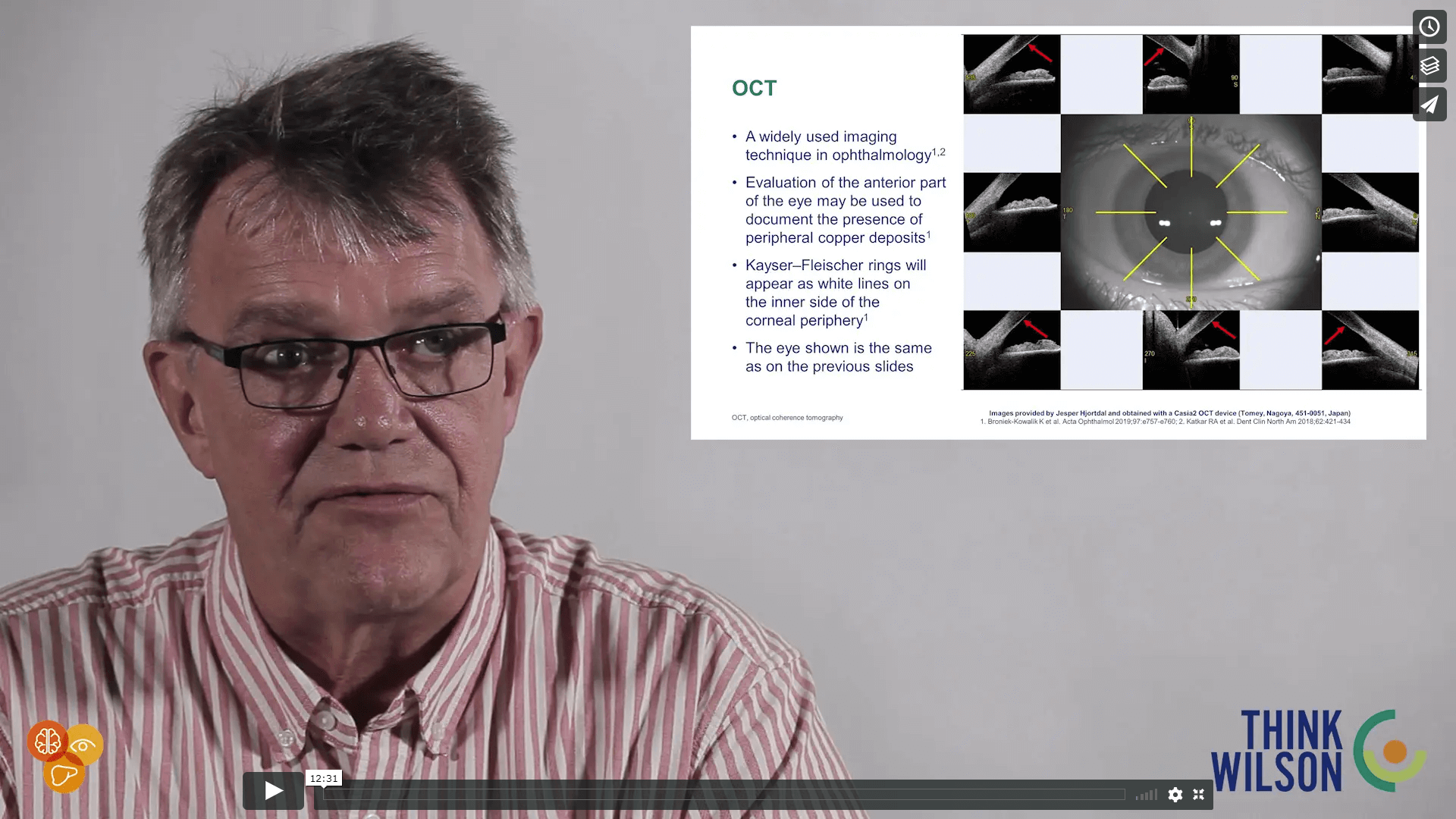
- Ophthalmologic
- Cardiovascular
- Cutaneous
- Hematologic
- Renal
- Gynecologic
- Musculoskeletal
Read on to learn more about the most common manifestations seen in patients with Wilson disease.
- Hepatic symptoms: reported as the initial clinical manifestation in ~61% (711/1172) of patients in an Austrian cohort studya,9
- In studies from neurology departments, 16–40% of patients present with hepatic symptomsb-d,8,10,11
- Neurologic or psychiatric symptoms: reported as the initial clinical manifestation in ~39% (461/1172) of patients in an Austrian cohort studya,9
- In studies from neurology departments, 59–82% of patients present with neurologic or psychiatric symptomsb-d,8,10,11
- Kayser–Fleischer rings: in cohort studies in Austria,9,12 China,10 and Germany,4 Kayser–Fleischer rings were present in ~80% (49/61) to ~98% (329/337) of patients with predominantly neurologic symptoms, and in ~27% (38/140) to ~52% (50/96) of patients with predominantly hepatic symptoms.a,d-f,4,9,10,12 However, Kayser–Fleischer rings are not entirely specific to Wilson disease as they can also be found in patients with chronic cholestatic liver disease and in children with neonatal cholestasis1,2